Virtual Reality in Diabetes Care: Beyond the Screen, Into the Self
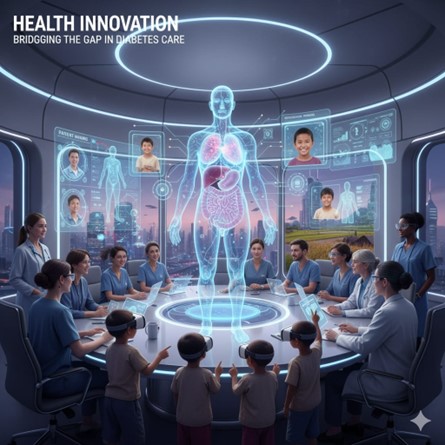
Virtual Reality and Interactive Care – The Future of Diabetes?
Imagine stepping into a world where learning to manage diabetes feels more like playing a really fun game than sitting through another lecture. For millions living with diabetes, education is crucial—but keeping patients engaged has always been a struggle. What if virtual reality (VR) could transform this experience, making diabetes care interactive, memorable, and even fun?
Yet the journey isn’t without its hurdles—VR must overcome barriers such as steep costs, limited accessibility, and a need for stronger clinical validation. Despite these obstacles, the technology sparks hope, unveiling a future where managing diabetes could be not just more effective, but genuinely enjoyable.
VR is becoming more common in healthcare due to engaging 3D visualization. It’s already being used successfully in many areas. A related technology, Digital Twin, is now being used alongside VR. It creates a digital copy of a patient or system to simulate real-time health conditions. This is especially useful for managing chronic diseases like diabetes, where patients’ needs can change daily.
Diabetes care requires regular monitoring and lifestyle changes. VR-based training and simulations can help patients better understand their condition and learn how to manage it. As diabetes cases grow faster than the number of specialists, these technologies offer easy solutions to improve patient education and self-care.
Virtual Reality-Based Diabetes Education for Clinicians
VR is emerging as a powerful tool in diabetes education, especially for training healthcare workers in rural areas, where access to certified diabetes specialists is limited and diabetes rates can be nearly double the national average.
A typical VR training scenario includes a realistic simulation of a hospital room with interactive nurse and patient avatars. Clinicians must recognize the symptoms and manage the condition appropriately.
This training approach offers a safe, controlled environment to practice managing diabetes emergencies. It also aims to improve clinicians’ cultural competency, confidence, and understanding of the latest therapies for diabetes. As the demand for diabetes care rises, VR can help primary care providers with the necessary skills to improve outcomes, particularly in underserved regions.
Virtual Reality Education for Adults with Diabetes in Rural Areas
VR is proving to be an effective educational tool for adults and children with diabetes, particularly in rural areas where health literacy is often lower, diagnosis is delayed, and access to diabetes specialists is limited—despite higher rates of diabetes.
The VR program includes interactive scenarios tailored to daily diabetes management. These range from safe exercise practices for people with diabetes in a virtual gym to carbohydrate counting in a virtual kitchen and glucose monitoring at work. Newly diagnosed individuals can also learn finger-prick testing in a realistic and supportive virtual environment.
The system delivers an evidence-based behavior change 
Because VR creates a strong sense of presence, it increases user engagement and focus, making learning more effective and memorable. This approach offers a scalable and accessible solution to support diabetes self-management, especially in underserved communities.
Virtual Reality-Based Education for Pediatric Diabetes Management
Emerging evidence suggests that VR is an effective tool for delivering nutrition and self-management education to children with diabetes. Interactive multimedia platforms, including VR, have been shown to significantly improve glycemic control, as evidenced by reductions in HbA1c levels, and enhance communication between pediatric patients and caregivers. However, due to the transient nature of educational effects, VR-based diabetes training should be administered at regular intervals to maintain efficacy.
Gamified VR environments offer an engaging and immersive educational experience, integrating healthcare content into interactive diabetes-related gameplay.
These environments can support behavior modification a
Virtual diabetes simulations allow users to practice self-care behaviors, complete knowledge assessments, and utilize personal treatment data, often alongside peer interaction through social media or multiplayer features. The use of virtual avatars and interactive games has demonstrated improvements in self-care behaviors, parent-child communication, and a reduction in diabetes-related emergencies.
Summary
In summary, VR serves as an effective tool for diabetes training, prevention, and treatment by offering immersive, risk-free learning for both clinicians and patients. It enhances disease understanding, promotes healthy behaviors, and expands access to quality care in advancing diabetes management.
Future VR systems for diabetes should be developed through collaboration among patients, clinicians, pharmacists, and educators to ensure practical, user-centered design. Incorporating community input will guide the creation of advanced VR tools that enhance training, management, and treatment for both adults and children with diabetes.
Reference: Virtual Reality Meets Diabetes – Neil Vaughan, 2025








